6. Complications, and reducing risk
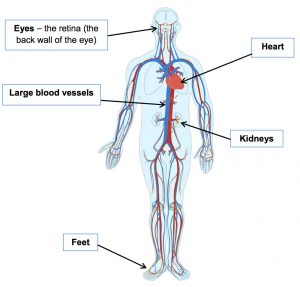
Diabetes can impact on many parts of the body by causing damage to the large blood vessels, small blood vessels and nerves.
Having high blood glucose levels, high blood pressure and high cholesterol can increase your risk and rate of damage. Smoking also damages blood vessels so will further increase your risk.
The parts of the body most often affected are:
Evidence has shown that people with Type 2 diabetes who manage their diabetes and achieve good levels of blood glucose, cholesterol and blood pressure control reduce their risk of developing complications.
Reducing the risk of loss of vision
 Regularly high blood glucose and high blood pressure can damage the small blood vessels at the back of the eye (the retina), this damage is called diabetic retinopathy. Damage to the retina can lead to reduced vision or blindness if it is not detected early and treated. The only way to check this is to have a digital photograph of the retina taken every year.
Regularly high blood glucose and high blood pressure can damage the small blood vessels at the back of the eye (the retina), this damage is called diabetic retinopathy. Damage to the retina can lead to reduced vision or blindness if it is not detected early and treated. The only way to check this is to have a digital photograph of the retina taken every year.
You will be sent a letter inviting you to attend for this along with a list of opticians who can take the photograph (this includes the community screening service held at the Manor Hospital). You will need to ring to make an appointment with the optician of your choice from this list.
Having the photograph taken does not replace the need for a full annual eye test with your own optician. If you have not received this letter within two weeks of diagnosis please contact your GP to check that you have been referred to the diabetic eye screening service.
Reducing the risk of heart disease (cardiovascular disease)
Diabetes speeds up the narrowing and hardening of the blood vessels (arteries) that occurs naturally through aging. Cholesterol, the main type of fat in the blood, can build up in the blood vessels making them more prone to blocking. If the large blood vessels to the heart, brain or feet get blocked this increases your risk of a heart attack, stroke or circulation problems to your legs or feet. You can reduce the risk of these complications by:
- Reducing the amount of fat in your diet
- Not smoking
- Taking regular exercise
- Reducing your weight (if overweight)
- Ensuring you attend your annual review appointment to have your blood pressure and cholesterol measured
Reducing the risk of damage to the nerves
Regularly high blood glucose levels can cause damage to nerves. Most commonly the nerves in the feet are affected. For men,nerve damage can result in not being able to get an erection. Good blood glucose control reduces the risk of nerve damage. If you have concerns about this, please talk to your healthcare professional.
Reducing the risk of kidney disease
Regularly high blood glucose and high blood pressure can cause damage to the small blood vessels in the kidney. This damage is called nephropathy which could eventually lead to needing dialysis. As part of your annual diabetes review your kidney function will be checked by a blood test and a urine test. Your blood pressure will also be checked as high blood pressure increases the risk of kidney damage. Often high blood pressure does not cause any signs or symptoms so it is very important to have your blood pressure checked at least once a year. If you are on medication for your blood pressure it will checked more often.
Gum disease
Gums can become damaged by high blood glucose levels and poor diabetes control can also lead to gum disease. Good control of blood sugars, healthy eating & stopping smoking can help reduce risk. Ensure your dentist is aware you have diabetes & attend regular dental check ups.
Reducing the risk of damage to the feet
Diabetes can cause:
- Nerve damage in the feet and legs resulting in altered sensation, pins and needles or possible numbness and burning sensations, this is called neuropathy.
- A reduced blood supply to the feet and legs resulting in cold, painful feet.
 This means that injuries to the feet may go unnoticed, be slow to heal and can quickly become infected.
This means that injuries to the feet may go unnoticed, be slow to heal and can quickly become infected.
It is important that your feet are examined as part of your annual review each year so that any problems can be treated early.
To prevent problems it is important that you care for your feet. The information on the next page should help you to do this.
- Wash your feet daily with a mild soap and luke warm water
- Dry your feet thoroughly, especially between the toes, using a soft towel or tissue
- For moist/sweaty skin between the toes apply surgical spirit with cotton wool
- To prevent dry skin use moisturising cream but avoid applying it between the toes
- When cutting your toenails follow the curve of the nail and avoid digging into the corners. Do not cut nails too short
- Use a pair of nail clippers and file the nails to avoid sharp edges
- For problem nails such as ingrown or thickened nails, or if you have poor eyesight, consult a HCPC Registered Podiatrist/ Chiropodist
- Corns and calluses should be dealt with by a podiatrist/chiropodist. Do not use razor blades, corn plasters etc. However you may use a pumice stone to smooth hard skin and corns
- Choose shoes with a fastening such as laces to hold the foot in place. Wear closed in shoes with a deep, round toe box to allow plenty of room for the toes.
- Have feet measured when buying new shoes. Always wear in new shoes gradually to prevent rubs/ blisters
- Avoid walking barefoot – always wear shoes/ slippers even indoors to protect your feet from injury
- Change your socks daily. Wear socks or stockings which fit correctly and are in good repair
- Look at your feet every day. Check between the toes and underneath your feet, you may need to use a mirror
- Things to look out for:
- Cuts, scratches and blisters
- Any change in colour (red, black, blue, white)
- Any changes in temperature between the feet
- Any discharge from a break or crack in the skin
- Any unusual swelling
- Painful areas
- If any of the above occur seek professional advice promptly.
- Check shoes inside and out before putting them on for cracks, pebbles or sharp edges which may irritate the skin. You may not be able to feel these if you have a loss of sensation
Annual review
To achieve the best possible state of health you need to work with the healthcare professionals.
You are entitled to have a full check up every year at your GP practice, this is called the annual review.
The annual review is very important as this is when the impact of your treatment is checked and any problems that are found can then be treated promptly.
At this review you should have the opportunity to discuss how you are coping with your diabetes and any problems or concerns you have. You will also be asked about your emotional wellbeing.
The review should include the following investigations:
| Test | Definition |
|---|---|
| HbA1c | Indicates blood glucose control over previous 3 months |
| Weight | Excess weight makes diabetes more difficult to control |
| Body Mass Index (BMI) | Equals weight in relation to height |
| Waist Circumference | Larger waist circumference can be linked to insulin resistance |
| Blood Pressure | Indicates how hard the heart has to work to move blood round the body |
| Blood Lipids: Total Cholesterol HDL LDL Triglycerides | Types of fat in the blood. HDL(High Density Lipoprotein is a good type of cholesterol). LDL(Low density Lipoprotein) & Triglycerides can be harmful to the heart and blood vessels |
| Kidney Function: Micro-albuminurea Serum Creatinine eGFR | Tiny amounts of protein in the urine, a higher level than normal can indicate early changes in the kidney Indicates level of waste products in the blood Indicates rate at which the kidneys are filtering the urine |
| Foot Examination | Checks circulation, sensation and condition of the feet |
| Retinal Photography | Photograph of retina (back wall of the eye) to check the condition |
If you are on insulin your injection sites should be examined.
At the end of the consultation you may have identified results that you wish to act on to reduce the rate/risk of diabetes complications.
Achieving your personal targets
You can use the forms on Appendix 1 (INSERT LINK) to record your personal targets and to record the results of your tests. It is recommend that you take this record to your appointments so that you can keep track of your progress.
| Which target do you want to act on? | How you could do it? | |
|---|---|---|
 |  |  |
| Reduce your blood glucose | Day to day ↑ physical activity ↓ sugary foods ↓ portion size of foods containing carbohydrate • Choose foods that turn into glucose slowly • Take medication as prescribed | Long term (insulin resistance) ↑ physical activity ↓ fat in diet ↓ saturated fat • Change to monounsaturated fats ↓ weight & waist measurement |
| Reduce your blood pressure | ↑ physical activity ↓ weight & waist measurement ↓ salt • Keep within advised alcohol limits • Stop smoking ↑ fruit & veg (5+/day) • Take medication as prescribed | |
| Reduce your cholesterol | ↑ physical activity ↓ fat in diet ↓ saturated fat • Change to monounsaturated fats ↑ fruit & veg (5+/day) • Take medication as prescribed | |
| Reduce your weight & waist measurement | ↑ physical activity ↓ fat in diet ↓ alcohol ↓ portion size of foods containing carbohydrate | |
| Stop smoking | Access smoking cessation programme via GP • Set a ‘quit’ date • Get support from family & friends • Nicotine replacement therapies | |
| Reduce depression | ↑ physical activity • Get support from family & friends • Talk to your GP • Access counselling/ other support via your GP • Take medication as prescribed |
Key:
↑ = increase
↓ = decrease
Thinking through the steps to achieving your target
Step1
Which target have you decided to work on?
E.g. reduce weight
Step 2
How could you do this? See above
E.g. ↑ physical activity
Step 3
Exactly how will you do this?
E.g. increase walking from 2 to 4 times a week
- What will you do?
E.g. start going for a 30 minute walk after evening meal
- When will you do it?
E.g. Tuesday and Thursday
Step 4
What might stop you doing this?
E.g. lack of motivation when weather is bad
Step 5
How might you overcome this?
E.g. planning to have company for the walk
Step 6
On a scale of 1 (no chance) to 10 (absolutely) how confident are you that you can do this?
If you rate your confidence at 5 or below you need to re think your plan, if you rate your confidence at 5-7 what would increase your confidence?
Step 7
Set a date to review your progress and set new targets.
Remember:
- What might seem like a small change can make a difference
- One action can affect several targets
- If you need support to achieve your target do not hesitate to talk to your nurse or GP
- There are several sources to go to for help
You can use the form in Appendix 1 (See Section 12) to record your targets and how you want to achieve them. It is recommended that you take this plan to your appointments to discuss with your healthcare professional.
